
If you weren’t paying close attention, you might have missed some big “noise” last week about coverage for hearing care.
A June 15 Centers for Medicare & Medicaid Services transmittal titled “Allowing Audiologists to Furnish Certain Diagnostic Tests Without a Physician Order” provided guidance for the finalized direct access policy that will allow beneficiaries, once every 12 months, to receive care for non-acute hearing assessments that are unrelated to disequilibrium, hearing aids, or examinations for the purpose of prescribing, fitting, or changing hearing aids.
As stated in the change request (CR) the purpose is to establish edits to ensure the following:
- That only one visit to an audiologist without a physician/NPP order is permitted, per beneficiary, once every 12 months, instructing that claims billed more frequently are denied;
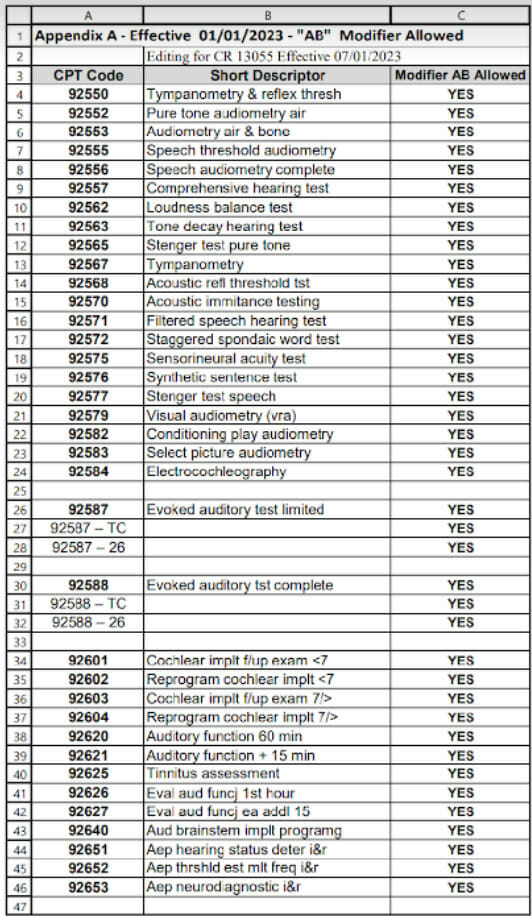
- That the visit may reflect one or more codes on an applicable list of 36 CPT codes, found in APPENDIX A, along with modifier AB, be billed via providers with certain bill types for outpatient hospitals, critical access hospitals, and SNFs; and,
- That an audiologist’s National Provider Identifier (NPI) is the rendering provider on the line of service, with the AB modifier, which is alongside an applicable code found in APPENDIX A.
The effective date of this change is July 1, 2023, with an implementation date of July 3, 2023.
So why is this such a big deal?
Mostly due to the daunting statistics on hearing loss in aging and the significant impacts on function and mention health. This change will increase access to care and allow for more proactive approaches to hearing health across the lifespan.
According to recent research, and as outlined in an article focused on hearing loss and aging from the American Speech-Language Hearing Association, the following are noted:
“Even using relatively narrow definitions, we can estimate that hearing loss affects up to 40% of adults more than 65 years old, 60% of adults over 75, and 80% of adults over 85 years” (Cruickshanks, Tweed, Wiley, Klein, Chappell, et al., 2003; Gates, Cooper, Kannel, & Miller, 1990; Reuben, Walsh, Moore, Damesyn, & Greendale, 1998).
Pretty significant numbers, right?
So how did we get to this point of allowing audiologist direct access?
As a history and background, audiologists are authorized to furnish diagnostic and balance assessment services under section 1861(ll)(3) of the Social Security Act (the Act).
Hearing and balance assessment services, termed audiology services, are generally covered as “other diagnostic tests” under section 1861(s)(3) of the Act. Audiology services may also be provided by physicians and non-physician practitioners (NPPs), including physician assistants (PAs), nurse practitioners (NPs), and clinical nurse specialists (CNSs) when authorized by state law and scope of practice.
Ok, so what is the recent change?
Before 2023, by regulation at 42 CFR 410.32(a), payment for all these diagnostic services furnished by audiologists were required to have an order from physicians or NPPs who are treating the patient. While all services furnished by audiologists must be personally provided, audiologists do not need the supervision of a physician/NPP to do so.
During Calendar Year (CY) 2023 Physician Fee Schedule (PFS) rulemaking, CMS finalized a regulatory provision at §410.32(a)(4) that allows an exception to the treating physician/NPP order requirement to allow audiologists to personally furnish certain diagnostic tests ─ using a finalized list of 36 Current Procedural Terminology (CPT) codes found in Table 36 in the CY 2023 PFS final rule at 87 FR 69662 ─ without an order.
Great! So what tests are we talking about?
Before you get too excited… these tests are limited to certain non-acute hearing conditions and diagnostic services related to implanted auditory prosthetic devices (including cochlear, osseointegrated, and auditory brainstem implants). But they may not include audiology services that are related to disequilibrium, or hearing aids, or examinations for the purpose of prescribing, fitting, or changing hearing aids (outlined at §411.15(d)).
Where can I find a list of the codes?
These services (including those that are listed as Audiology Services not requiring a physician/NPP order, as applicable, on the PFS website) may be performed once every 12 months using modifier AB created for this purpose.
How is the AB modifier defined?
AB ─ its long descriptor: Audiology service furnished personally by an audiologist without a physician/NPP order for non-acute hearing assessment unrelated to disequilibrium, or hearing aids, or examinations for the purpose of prescribing, fitting or changing hearing aids; service may be performed once every 12 months, per beneficiary.
So, in closing, what should SNF providers know about this benefit?
To begin, don’t assume that the implanted auditory prosthetic devices means you don’t need to know about these services.
According to the American Speech-Language Hearing Association as of December 2012, it was estimated that, in the United States, approximately 38,000 devices have been implanted in children and 58,000 devices have been implanted in adults, with an estimated 324,200 devices implanted worldwide (National Institute on Deafness and Other Communication Disorders, 2016).
Engage with audiology professionals in your communities to determine the best opportunities for responsible use of these allowances for those we serve.
Here’s a full list of allowable CPT codes below for reference:
Renee Kinder, MS, CCC-SLP, RAC-CT, is Executive Vice President of Clinical Services for Broad River Rehab. Additionally, she serves as a member of American Speech Language Hearing Association’s (ASHA) Healthcare and Economics Committee, is a member of the University of Kentucky College of Medicine community faculty and is an advisor to the American Medical Association’s Current Procedural Terminology CPT® Editorial Panel. She can be reached at [email protected]
The opinions expressed in McKnight’s Long-Term Care News guest submissions are the author’s and are not necessarily those of McKnight’s Long-Term Care News or its editors.
Have a column idea? See our submission guidelines here.




